Dental procedures, especially extractions, often precipitate a flurry of insights and concerns among patients about post-operative care. One pertinent topic frequently encountered after such procedures is the phenomenon known as dry socket. This condition, medically referred to as alveolar osteitis, is characterized by an unbearable pain that occurs when the blood clot within the socket fails to develop or becomes dislodged. A common inquiry in this realm pertains to the use of stitches—commonly known as sutures—post-extraction and whether they relate to the development of dry socket. This exploration seeks to demystify the relationship between stitches and the risk of dry socket.
Understanding Dry Socket
Before delving into the association between stitches and dry socket, it is essential to comprehend what dry socket entails. Following a tooth extraction, particularly the removal of wisdom teeth, a blood clot forms in the vacant socket. This clot is crucial; it acts as a biological bandage, protecting the underlying bone and nerves while paving the way for proper healing. Should this clot dislodge or fail to form adequately, it exposes the bone and nerves, leading to significant discomfort and healing complications.
Dry socket manifests typically three to five days post-extraction, with symptoms including a piercing pain that often radiates towards the ear, eye, or temple, halitosis, and an empty-looking socket with a visible bone. The quest for relief may lead individuals to seek answers, particularly regarding their surgical care.
Defining the Role of Stitches
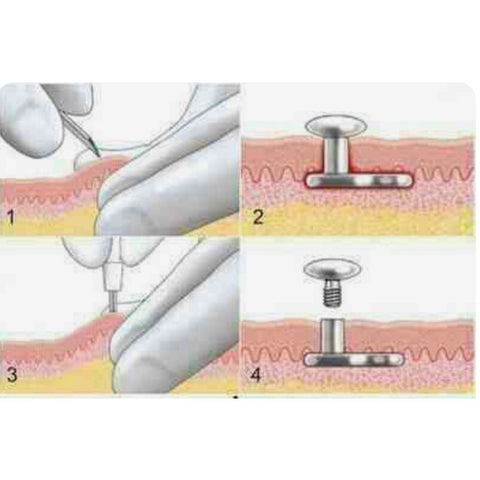
Sutures are employed in various dental procedures, primarily to help secure the soft tissues back together post-extraction. The primary function of stitches is to encourage the soft tissues to heal effectively, reducing the risk of complications such as infection or improper healing. Stitches can be either dissolvable or non-dissolvable, with each type serving its purpose in the healing process. Once placed, stitches can stabilize the area, theoretically minimizing movement that could dislodge a blood clot.
Can You Get Dry Socket With Stitches?
The direct answer is yes; it is entirely possible to experience dry socket even if stitches are present. Stitches do mitigate certain risks associated with the healing process, but they do not eliminate the possibility of dry socket. The formation of a proper blood clot is critical, regardless of whether or not stitches have been applied. Various factors influence the occurrence of dry socket:
- Type of Extraction: Some extractions, especially those of impacted molars, bear a higher risk of dry socket, irrespective of stitches.
- Patient Habits: Smoking, vigorous rinsing, or spitting post-surgery can disrupt clot formation. Actions that create suction in the mouth may lead to clot dislodgement.
- Pre-existing Conditions: Certain health conditions, such as diabetes or autoimmune disorders, can complicate healing processes, making the development of dry socket more likely.
Factors That May Increase the Risk of Dry Socket
The complexity of the mouth’s healing environment necessitates a nuanced understanding of factors contributing to dry socket. Beyond the presence of stitches, several other elements can exacerbate the likelihood of developing this painful condition:
- Age: Research indicates that younger patients may be more susceptible to dry socket, particularly those in their late teens or early twenties.
- Hormonal Variations: Women who are menstruating or taking oral contraceptives could be at an increased risk due to hormonal influences on healing.
- Trauma to the Site: Any additional trauma incurred during surgery or afterwards can compromise the integrity of the blood clot.
Post-Operative Care and Prevention
Recognizing that dry socket can still occur even with stitches, it is critical to employ meticulous post-operative care to enhance healing and minimize risks. Here are some proactive measures to consider:
- Follow Instructions: Adhere strictly to the dentist or oral surgeon’s post-op instructions, including dietary restrictions and activity levels.
- Avoid Smoking: Steer clear of smoking or using nicotine products for at least 72 hours as these can disrupt healing.
- Gentle Oral Hygiene: Maintain a robust oral hygiene regimen but avoid vigorous rinsing. Consider using a saline solution for gentle rinsing rather than commercial mouthwashes.
- Avoid Hard Foods: Stick to soft foods, avoiding anything that may require excessive chewing or that can potentially dislodge the blood clot.
Conclusion
In summary, while stitches play a vital role in ensuring the proper healing of the extraction site, their presence does not deter the risk of dry socket. Understanding the intricate interplay between post-operative care, the factors influencing healing, and the possibility of this painful condition is paramount for patients. Careful adherence to aftercare guidelines combined with a keen awareness of one’s habits can significantly diminish the risk of dry socket and foster a smoother healing process. Knowledge empowers, and by educating oneself regarding these intricacies, patients can navigate the post-operative period with greater confidence and comfort.





Leave a Comment