Gum disease, a pervasive and often underestimated condition, engenders a multitude of concerns not only for personal health but also for broader implications regarding systemic wellness. At first glance, the question “Does gum disease kill you?” might seem overly dramatic. However, as awareness grows about the interconnectivity of oral health and overall bodily function, the inquiry reveals a richer tapestry of relationships worthy of exploration.
To delve deeper into this examination, it is essential to understand the dual nature of gum disease, also known as periodontal disease. Broadly categorized into gingivitis and periodontitis, this condition manifests through inflammation, infection, and the potential for severe dental and health repercussions. While most individuals experience some degree of gum inflammation as they age, persistent or severe forms can lead to life-threatening situations. This article endeavors to elucidate the deeper significance of gum disease, highlighting its potential dangers and systemic effects, while ultimately answering the crucial question of its lethality.
1. Understanding Gum Disease: The Fundamentals
At its core, gum disease represents the body’s inflammatory response to harmful bacterial accumulation. Poor oral hygiene enables plaque—a sticky film of bacteria—to form on teeth, leading to inflammatory reactions of the gums. Gingivitis, the milder form, is characterized by symptoms such as redness, swelling, and occasional bleeding during brushing. It’s often reversible with diligent oral care.
However, when left untreated, gingivitis can develop into periodontitis, a severe infection that erodes gum tissue and can lead to tooth loss. The inflammation progresses down to the bone supporting the teeth, which can create pockets of infection and even systemic complications.
2. The Hidden Link: Oral Health and Systemic Illness
Recent studies have illuminated the intricate connections between oral health and systemic diseases. The mouth serves as a gateway to overall health, and gum disease has been associated with a slew of chronic conditions, including diabetes, heart disease, and even respiratory ailments. With a myriad of bacteria residing in the oral cavity, periodontal disease facilitates the translocation of these pathogens through the bloodstream, impacting distant organs.
For instance, individuals with gum disease have been observed to experience higher rates of cardiovascular incidents. The inflammatory markers produced as a result of periodontal infection may contribute to vascular inflammation or arterial plaque formation, thereby exacerbating heart health issues. This burgeoning field of research has positioned gum disease as more than a dental nuisance, casting it in a more sinister light as a potential harbinger for broader health crises.
3. Risk Factors: Who is Prone?
The susceptibility to gum disease is influenced by several intrinsic and extrinsic factors. Age emerges as a significant determinant; older adults are particularly affected due to cumulative exposure to periodontal pathogens and the fragility of supporting tissues. Additionally, genetic factors can predispose individuals to greater susceptibility, as certain genetic profiles may elicit heightened inflammatory responses.
Lifestyle choices—such as smoking, poor nutrition, and inadequate oral hygiene—also play pivotal roles. Smoking, in particular, is a notorious risk factor, significantly reducing blood flow to the gums and impairing healing processes. A diet rich in sugary and acidic foods promotes plaque build-up and accelerates gum disease progression. Those with pre-existing health conditions like diabetes or autoimmune disorders face compounded risks, making effective oral care even more perilous.
4. The Dangers: Does Gum Disease Kill You?
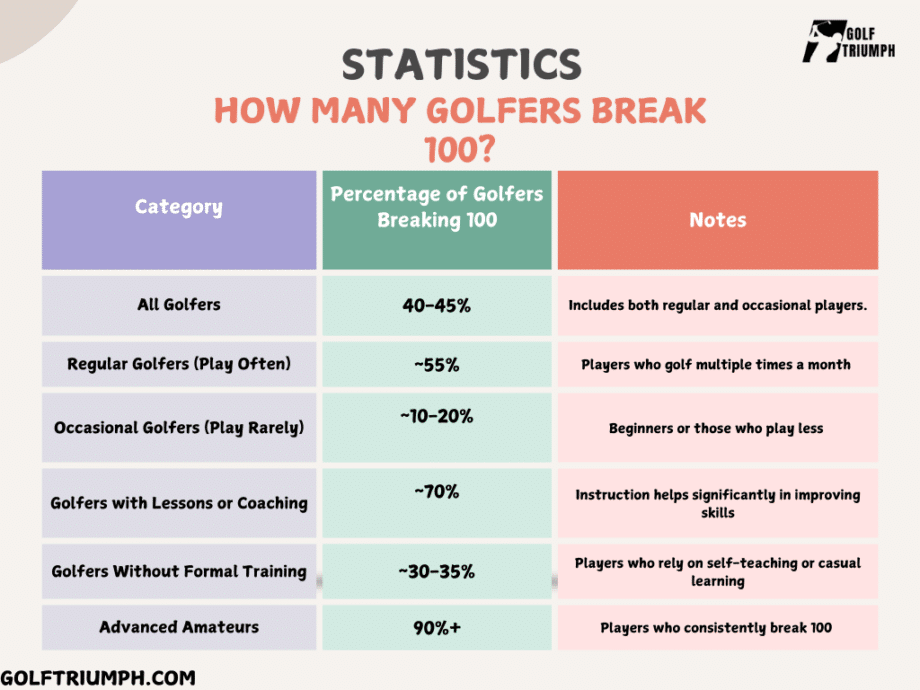
Addressing the crux of the query regarding gum disease’s lethality reveals a multi-faceted answer. While it’s rare for gum disease to be the direct and sole cause of death, its manifestations can significantly contribute to life-threatening conditions. Complications arising from untreated infections can lead to sepsis, a severe systemic response to infection that can be fatal.
Moreover, the indirect consequences of gum disease—through its associations with chronic diseases—can lead to an elevated mortality risk. Studies suggest that individuals with chronic periodontal disease face a greater likelihood of dying from heart disease, strokes, and diabetes-related complications. These statistics reveal how gum disease could be seen as a significant risk factor in a continuum of health maladies rather than an isolated concern.
5. Prevention and Management: Steps to Take
Preventing gum disease and its associated risks entails a holistic approach to oral care. Regular dental check-ups are vital for early detection and intervention. Individuals should engage in daily brushing and flossing, minimizing plaque accumulation. Adopting a nutrient-rich diet that supports gum health, while steering clear of tobacco and excessive sugar, further fortifies one’s defenses against gum disease.
For those already grappling with gum disease, professional treatments including deep cleanings, scaling, and root planing may be necessary. In more advanced situations, surgical interventions may be warranted. Importantly, patients should adopt a proactive stance, recognizing the intricate links between oral health and overall wellness, fostering conversations with dental professionals about any symptoms or concerns.
In conclusion, the query regarding whether gum disease can kill is less about a definitive answer and more about understanding the broader health implications associated with poor oral hygiene. While the disease may not be a direct killer, it serves as a potent reminder of the interconnected nature of bodily health. By prioritizing oral hygiene, individuals can not only preserve their dental health but also bolster their overall well-being, steering away from the hidden dangers lurking beneath the surface of gum disease.









Leave a Comment